| STAGE | FINDINGS |
|---|---|
| 1 | Eccentric steepening Myopia, induced astigmatism, or both <5.00 D Mean central K readings <48 D |
| 2 | Myopia, induced astigmatism, or both from 5.00 to 8.00 D Mean central K readings <53.00 D Abscence of scarring Corneal thickness >400 micron |
| 3 | Myopia, induced astigmatism, or both from 8.00 to 10.00 D Mean central K readings >53.00 D Abscence of scarring Corneal thickness 300 – 400 micron |
| 4 | Refraction not measurable Mean central K readings >55.00 D Central corneal scarring Corneal thickness < 200 micron |
Keratoconus
Keratoconus & Noninflammatory Ectatic Disorders
Keratoconus
✦ Kerato= Horn, cornea
✦ Conus= cone
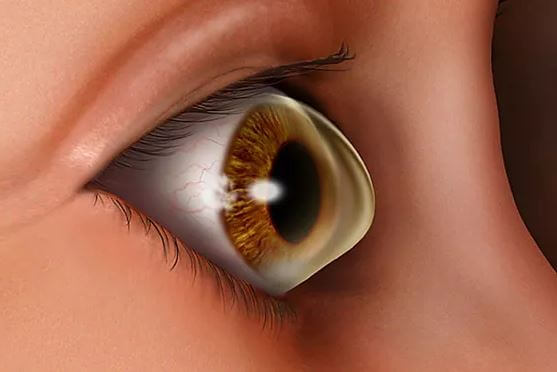
✦ Keratoconus is a noninflammatory , ectatic corneal condition characterized by central or paracentral stromal thinning , apical protrusion and irregular astigmatism
✦ British physician, Jhon Nottingham in 1854 did practical observations on conical cornea
✦ 50-230 / 100000 individuals
✦ M=F
✦ Starts at puberty, over a period of 10 to 20 years the process continues until the progression gradually stops
✦ Familial incidence= 65%, Autosomal dominant with variable penetrance
✦ Pathophysiology:
✤
Antioxidant
deficiency
✤ Proteinase and antiproteinase imbalance: up-regulation of degradative enzymes and the down-regulation of proteinase inhibitors could result in a degradation of the extracellular matrix of the stroma
✤ Apoptosis: Keratocytes from keratoconus corneas have been found to have four times the interleukin-1 binding sites, when compared to nonkeratoconus corneas. This may result in an increased sensitivity of the keratocytes in keratoconus to the effects of interleukin-1. Interleukin-1 has also been shown to induce apoptosis or controlled cell death of stromal keratocytes in vitro.
✤ Contact lens wear is another form of corneal microtrauma: 17.5% to 26.5%
✤ ectodermal disease, then associations with atopic disease and tapetoretinal degenerations
✦ Pathology:
✤ Breaks in the epithelial layer can be associated with epithelium growing posteriorly into Bowman's layer and collagen growing anteriorly into the epithelium, forming Z-shaped interruptions at the level of Bowman's layer. These Z-shaped areas are typical of keratoconus.
✤ Fleischer ring found at the base of the cone
✤ normal-sized collagen fibers; however, the number of collagen lamellae was abnormally low. The number found within the cone was less than half (41%) the number outside of the cone.
✤ Endothelial cell pleomorphism and polymegathism occur in keratoconus
✦ Clinical Features:
✤ Late teens
✤ Blurring of vision
✤ Shadowing around images
✤ Glare, halos, ocular irritation
✤ Frequent changes in spectacle number
✤ Contrast sensitivity measurement may, however, uncover visual dysfunction before Snellen visual acuity loss can be measured
✤ Two types of cones have been described. The round or nipple-shaped cone is smaller in diameter, while the larger oval or sagging cone may extend to the limbus and is more prone to contact lens fitting problems.
✦ Signs:
✤ Irregular astigmatism
✤ Striae occur in the posterior stroma, just anterior to Descemet's membrane.
✤ Red reflex Oil droplet sign
✤ Scissoring reflex
✤ Vogt ‘s straie
✤ Fleischer’s ring
✤ Prominent corneal nerves
✤ Corneal topograph
✤ Progressive corneal thinning
✤ Munson’s sign
✤ Central corneal scarring: Factors predictive of incident corneal scarring include corneal curvature greater than 52 diopters (D), contact lens wear, corneal staining, and age less than 20 years.
✦ From Fruste Keratoconus (FFKC) was originally described by Prof. Marc Amsler (1891-1961) based on reflection Placidodisk photography, prior to the development of computerized corneal imaging technologies. FFKC was used to describe an abortive form of the disease that may progress or may not.
✦ Investigations:
✤ The keratometer is an invaluable, widely available tool for measuring corneal curvature. Inability to superimpose the central keratometric rings suggests irregular corneal astigmatism, a hallmark of keratoconus.
✤ Keratoscopy or videokeratography, based on the Placido disk, can provide qualitative contour information. In early keratoconus, a focal area of increased corneal curvature appears as an isolated area of smaller ring spacing and distortion. As the condition progresses, the ring spacing decreases overall and becomes increasingly irregular
✦
Rabinowitz has suggested four quantitative videokeratographic indices as an aid for screening patients for
keratoconus. These indices include
1.
Central corneal
power value greater than 47.2 D
2.
Inferior–superior
dioptric asymmetry (I-S value) over 1.2
3.
Sim-K
astigmatism greater than 1.5 D
4.
Skewed
radial axes (SRAX) greater than 21 degrees.
✦
Indices
✤ Simulated keratometry (SimK)
✤ Surface asymmetry index (SAI):
✤ Asymmetric bow tie (AB) with skewed radial axes (SRAX): Skewing of more than 30° is described as significantly abnormal
✤ Rabinowitz/Mc Donnel diagnostic criteria consists of two topography derived indices, which are as follows;
▪ Central K-value > 47.20 D and
▪ Inferior-Superior asymmetry (I-S value) > 1.4 D
✤ Rabinowitz/Rasheed’s described KISA% index:
▪ Uses 4 parameters →
▪ Keratometry; I-S value; the AST index, which quantifies the degree of regular corneal astigmatism (simulated flat and steep keratometry values, Sim K1 and Sim K2); and SRAX, which is an expression of irregular astigmatism.
▪ KISA% > 100% is considered as highly suggestive of keratoconus.
✤
Keratoconus-prediction
index(KPI) → Indices of Maeda and
Klyce
▪ Derived from eight other quantitative videokeratographic indices.
▪ Two simulated K values (steep and flat powers), differential sector index (DSI), center/surround index (CSI), opposite sector index (OSI), surface asymmetry index (SAI), analyzed area (AA), and the irregular astigmatism index (IAI).
Amsler-Krumeich Classification for Keratoconus
Keratoconus Severity Score (KSS) Ranking Scheme
| Grade | Stage | Corneal scarring* | Slit-lamp signs* | Axial Pattern | Other Features |
|---|---|---|---|---|---|
| 0 | Normal topography | None | None | Typical | Average corneal power (ACP) ≤ 47.75 D, Higher-order RMS error** ≤ 0.65 |
| 1 | Atypical Topography | None | None | Atypical: - Irregular -Sup. bowie -Inf. bowie -Inf. or Sup. area of steepening no more than 3.00 D steeper than ACP | ACP ≤ 48.00 D, Higher-order RMS error ≤ 1.00 |
| 2 | Suspect Topography | None | None | Isolated area of steepening: -Inferior -Superior -Central steep | Additional features: ACP ≤ 49.00 D or Higher-order RMS error > 1.00, ≤ 1.50 |
| 3 | Mild disease | None | Possible | Consistent with KCN | Additional features: ACP ≤ 52.00 D or Higher-order RMS error > 1.50, ≤ 3.50 |
| 4 | Moderate disease | Add features: Corneal scarring and overall CLEK grade up to 3.0 | Possible | Consistent with KCN | Additional features: ACP > 52.00 D, ≤ 56.00 D or Higher-order RMS error > 3.50, ≤ 5.75 |
| 5 | Severe disease | Add features: Corneal scarring CLEK grade 3.5 or greater overall | Must have | Consistent with KCN | Additional features: ACP > 56.00 D or Higher-order RMS error > 5.75" |
✦ ABCD Classification: The ABCD classification is measured at the cone.
✤ A: Anterior radius of curvature from a 3.0-mm zone centered on thinnest point
✤ B: Posterior (back) radius of curvature from a 3.0-mm zone centered on the thinnest point
✤ C: Minimal corneal thickness (not apical)
✤ D: Best spectacle-corrected visual acuity
✦
Systemic
Association:
✤ ATOPY
▪ Asthma
▪ Atopic keratoconjunctivitis
▪ Hay fever
▪ Eczema
✤ CONNECTIVE TISSUE DISORDERS
▪ Marfan’s syndrome: An increased prevalence (38%[20] to 58%) of mitral valve prolapse has been found in keratoconus patients
▪ EDS
▪ Osteogenesis imperfecta
✤ MISCELLANEOUS
▪ Down’s: 5.5% and 15%
‣ structural or biochemical changes
‣ habitual eye rubbing
▪ Turner’s syndrome
✤
Diabetes
offered a protective effect regarding keratoconus. (also smoking?? As they
cause C3R like effect)
✦
Ocular
Associations:
✤ RP
✤ Infantile tapetoretinal degeneration (Leber's congenital amaurosis) is frequently complicated by keratoconus and cataract.
✤ retinopathy of prematurity, progressive cone dystrophy, aniridia, iridoschisis, and essential iris atrophy
✤ VKC: 26.8%.
✤ 17% in a group of patients with floppy eyelid syndrome.
✦ Complications:
✤ High Refractive errors: Intolerance to glasses
✤ Acute Hydrops : Rupture Descemet’s membrane → Aqueous influx → Corneal edema → Sudden drop in vision / Opacity
✦
Keratoconus
Progression
✤ K-max (steepest keratometry) ≥ 1 D increase
✤ K-max – K-min ≥ 1 D increase (K-min, flattest keratometry)
✤ Kmean ≥ 0.75 D increase (Kmean = average of K-max K-min)
✤ Pachymetry ≥ 2% decrease in central corneal thickness (CCT)
✤ Corneal apex power ≥ 1 D increase (measured with cone location and magnitude index)
✤ MRSE change ≥ 0.5 D
✤ Several established decision trees exist based on combinations of the above, such as the Klyce indices of Surface Asymmetry Index (SAI) and Surface Regularity Index (SRI) and KISA% Index.
Management
✦ The management of keratoconus begins with spectacle correction.
✦ Once glasses fail to provide adequate visual function, contact lens fitting is required. Contact lens wear improves visual function by creating a new anterior refractive surface. Contact lenses do not prevent progression of corneal ectasia. While they seem to be associated with the development of keratoconus in some cases, this important mode of therapy should never be withheld for fear of causing progressive disease.
✤ RGP: three-point touch technique, remain the mainstay of contact lens treatment for keratoconus. apical clearance fitting technique is also commonly used.
✤ Other options include soft toric lenses, standard bicurved hard lenses, custom-back toric lenses, piggyback systems, hybrid lenses made of combined hard lens with a soft skirt, scleral lenses, and mini-scleral lenses.
✤ Silicone-hydrogel (Si-Hy) lenses, keratoconus designs
✤ Hybrid lenses, such as the SoftPerm lens (CIBA Vision Corp., Duluth, GA) and the newer SynergEyes KC lens (SynergEyes, Inc., Carlsbad, CA) may be more comfortable for patients who cannot tolerate an RGP alone.
✤ Mini-scleral lenses have a diameter of 14–17 mm compared to scleral lenses with a diameter of 20–24 mm.
✤ PROSE (prosthetic replacement of the ocular surface ecosystem): A medical model
✤ Outcomes
▪ Bigger is better. Size matters.
▪ There is no cone that cannot be fit.
▪ Scleral lens is an option after hydrops.
✤ New Paradigm for Contact Lens in Keratoconus
▪ Not a “contact lens failure” without trial of “true” scleral lens > 18 mm
▪ Penetrating or lamellar keratoplasty only for axial opacity limiting vision (in specialty lens)
▪ No regraft for cylinder or recurrence of ectasia without trial of specialty lens
▪ New Si-Hy lenses with keratoconus designs have extended the use of soft lenses in keratoconus.
▪ New hybrid materials and designs address past failures from lens fragility and hypoxia.
▪ Scleral lenses are in the repertoire of an increasing number of specialty lens fitters.
▪ Scleral lenses are a useful option in cases of RGP corneal lens failure due to instability or tight lens syndrome.
▪ The definition of scleral lenses is evolving. “Miniscleral,” corneoscleral, and intralimbal lenses may not perform as well as scleral lenses.
▪ PROSE treatment is a good option for contact lens and even scleral lens failures and can accommodate any cone.
▪ PROSE treatment has favorable 1-year outcome in comparison to keratoplasty for moderate to severe keratoconus.
✦ Contact lens-intolerant keratoconus patients without central scarring, who have mild or moderate disease, may be candidates for intrastromal ring segment insertion. The ideal candidates also have low spherical equivalents and average keratometry readings of less than 53 D.
✤ Ferrara rings (Ferrara Ophthalmics, Belo Horizonte, Brazil) and Intacs (Addition Technology Inc, Des Plaines, IL, USA), commonly used ring segments, are made of rigid polymethyl methacrylate. Ferrara rings have a fixed inner diameter of 5.0 mm and a triangular anterior contour. Intacs have an inner diameter of 6.8 mm, a flat anterior surface, and are available in thicknesses of 0.25–0.45 mm, in 0.05 mm increments.
✦ C3R
✦ While penetrating keratoplasty has traditionally been the surgery of choice, lamellar surgery is becoming more popular for patients with mild to moderate disease.
✤ The iron ring, found at the base of the cone, should be used as a reference when planning graft size.
✤ Postkeratoplasty myopia can be reduced by using the same-sized donor and host corneal buttons.
✦
Lamellar
Keratoplasty
✤ Deep anterior lamellar keratoplasty (DALK): host endothelium is preserved, thus reducing the risk of rejection. The risk of endophthalmitis is theoretically less because this is largely an extraocular procedure.
✦ Corneal Allogenic Intrastromal Ring Segments (CAIRS) Combined With Corneal Crosslinking for Keratoconus
✤ Under study
✤ CAIRS trephined from donor cornea using a double-bladed trephine were implanted into mid-depth femtosecond laser– dissected channels in the cornea of patients with keratoconus in the 6.5-mm optic zone, followed by accelerated corneal crosslinking (A-CXL)—either conventional or contact lens–assisted CXL (A-CACXL), depending on minimum corneal thickness.
- compiled & published by Dr Dhaval Patel MD AIIMS
